OROFACIAL PAIN AND DISORDERS
Orofacial pain and disorders, sometimes called
TMJ or TMD, are often associated with some of the following classical
signs and symptoms:
- Headaches
- Clicking and/or popping noises in either one or both jaw joints
- Clenching
- Grinding - bruxing teeth at night-time, or even during the daytime
- Dizziness
- Fatigue
- Cramps and pains in the face and/or neck
- Limited mouth opening
- Inability to chew effectively
- Loss of back teeth
- Improper bites
- Loss of hearing
- Tinnitus
- Poor body posture
- Difficulty talking
- And, prior orthodontic treatment;
where any one or more may indicate a
problem.
In order to properly diagnose these disorders
many steps must be taken to ascertain a positive cause and effect
relationship through signs and symptoms. The patient is a valuable
source of information in this regard, as the symptoms - the
information the patient gives - is solicited by questionnaires,
and direct discussions. The signs come from many examinations of the
patient to include:
Muscle exam
where muscles along with their origins and
insertions on bones are palpated for: pain, tender points, tonicity,
reflexes, and trigger points.
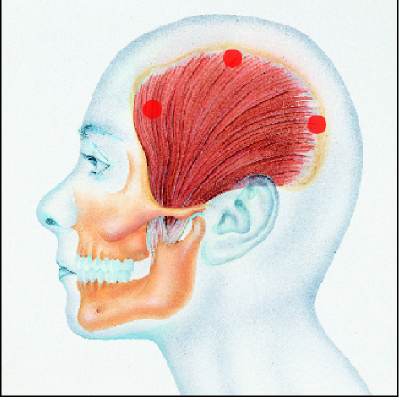
The temporalis muscle covers the side of the
head, and is actually three muscles in one, as each portion of the
muscles contracts at a different time dependant on the jaw movement.
This muscle is attached to the lower jaw in front of the jaw joint,
which acts like a hinge. When the temporalis contract the lower jaw is
elevated until all the teeth touch. Where this muscle attaches to the
lower jaw by many tendons pain is often solicited, much like tennis
elbow. When the patient feels a headache coming on, massaging this area
inside the mouth by the thumb and the outside by the middle finger,
often make the headache goes away immediately. There are many
reasons why this muscle induces headaches, which can be determined by
the exams.
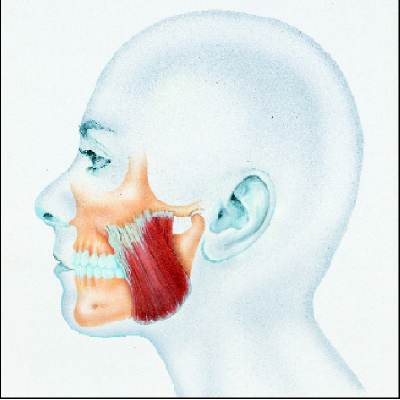
This
image shows the big masseter [cheek] muscle used in chewing, by
elevating the lower jaw. In humans this muscle does most of the
work, it has two portions each with different functions, and its
origin on the cheek bone can refer pain such as headache.

Like
all bones being moved by muscles, the lower jaw bone is no exception
regarding the two contrasting groups of muscles performing the
movements. While there are many muscles that elevate the lower jaw
for chewing, talking and augmenting breathing, there are many muscles
acting in opposition to the elevating [closing] muscles that lower
the lower jaw. These muscles can cause improper head posture, and
they can also refer pain to the head. Some of these muscles attach
to the voice-box, and are required in proper swallowing.
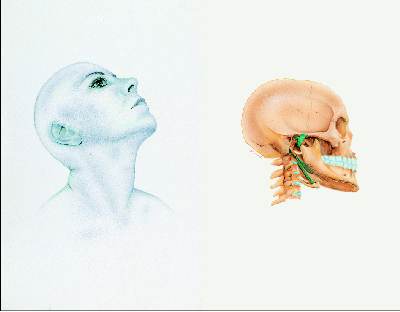
Posture exam
where the posture of
the entire body is assessed for alignment, because often forward head
posture caused by a lack of what is called - vertical dimension
- which is the amount the lower jaw is postured away from the
upper jaw when the patient bites on all teeth. An over-closed lower
jaw causes the head to rotate forward, and because the eyes
involuntarily always keep the head horizontal to the horizon, the
head moves forward. This results in improper alignment of the
cervical spine - the neck bones, and makes the muscles
supporting the head do unnecessary work, often leading to pain in the
neck muscles. The body's skeleton further compensates for the
head and neck being out of position, by creating a lordosis -
curve, of the lower back. This results with the pelvis rotating, and
then further compensation is created by the locking of the knees.
This is further compensated by rotating of the ankles
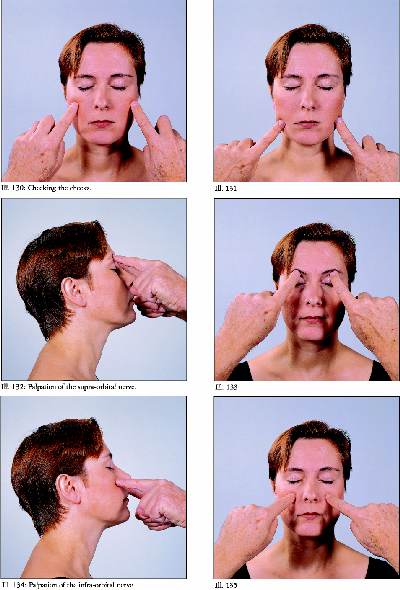
Sensory and Motor nerve exam
This exam is accomplished by palpation of the
foramen - holes, in the head bones where these nerves exit from the
brain case.
Tooth Status
The
routine examination of the teeth directly with the aid of radiographs
is also required to determine if there are any associations between
the status of the teeth, the bone housing the teeth and the gingival
tissues covering these bones and surrounding the teeth, with the pain
the patient is experiencing. Anyone having a tooth ache knows that
the pain associated with a diseased tooth effects the entire side of
the face.
Occlusal Gram exam
During this examination the manner in which the teeth
come together in the closed position as well as the various contacts of
the teeth when the lower jaw is moved from side to side is charted.
Sometimes teeth interfering with the normal functional movements of the
lower jaw place undue pressure in the jaw joints causing pain in the
joints and related muscles.

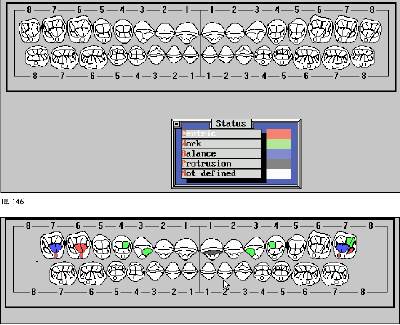
The completed occlusal gram gives indications
of whether or not a few or many teeth actually touch, how many tooth
surfaces actually participate in chewing, the presence of undesirable
balancing contacts and whether or not the front teeth are functioning
properly.
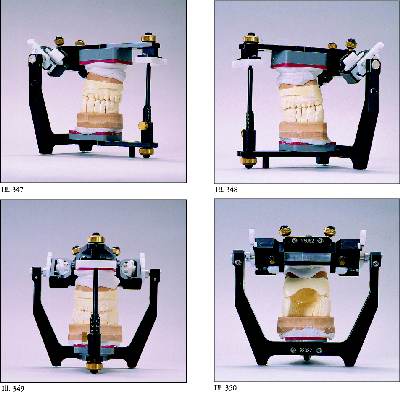
Diagnostic Casts exam
Impressions are made of
the patient's teeth, and the casts of the teeth are related to each
other by using a reference position bite relationship. The upper cast
is mounted to an instrument called an articulator by either an anatomic
or hinge axis face bow, which relates the casts of the patient's teeth
to the jaw joints. The articulator can be set to reproduce the
patient's lower jaw movements from the computerized Condylographic
data. Because the patient's teeth are now represented in a dynamic
movement fashion, determinations can be made on how the teeth actually
function in the mouth, and especially how the teeth dominate the
position of the jaw joints. The specialized casts shown here allow
for the evaluation of individual teeth, as all the posterior [back]
teeth can be removed from the cast, and replaced one at a time.
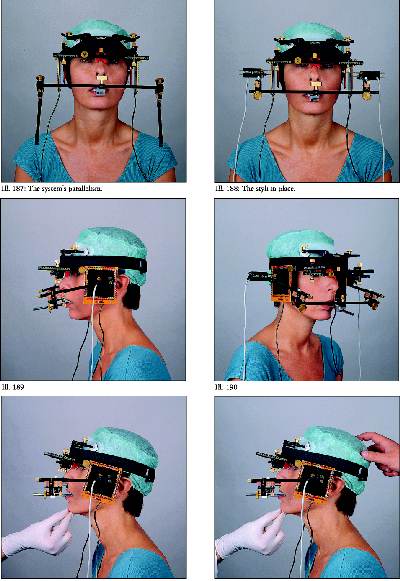
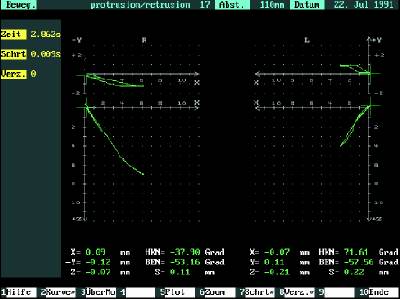
Condylographic exam
there are two
computerized devices which give representations of how the jaw joints
are working, and their specific pathways are related mathematically by
two graphs for the right and left forward - backward movements, and two
graphs for the sideways movements. The more simplified computerized
system enables this information to be obtained in eight minutes. From
the graphs of the patient's jaw joint movements, determinations of
health status of each jaw joint can be deduced. When observations are
made which don't appear normal, a more extensive computerized system
is used to make more finite observations of not only each jaw joint
but also the relationships of the jaw movements to all the teeth.
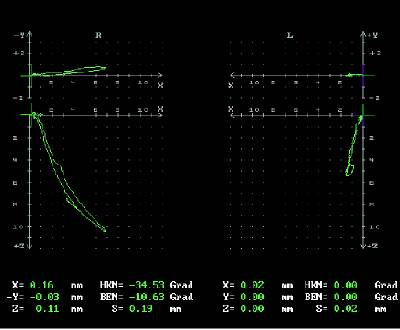
This diagram from Condylography shows the
pathways of the right and left jaw joints. Data is also given in
hundredths of a millimeter and seconds at each point along this pathway.
In this case, the patient's left jaw joint is restricted, making the
right jaw joint compensated for this lack of mobility in the left jaw
joint.
In this 50 year old patient, the left joint
shows a remarkable shift when the jaw is moved along with highly
restricted movement, indicating a problem within the jaw joint
itself.
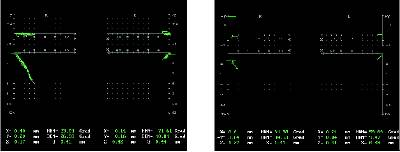
In this case the patient favors the left side and the patient has atypical jaw movements
when chewing and speaking.
This case shows the disc is out of place
The spike in the time of movements on the left side when the teeth are
shown the extreme velocity of the jaw touching and then the disc goes to
where movement when disc goes to place is should be on the condyle when
the mouth is opened and is termed a reciprocical click.
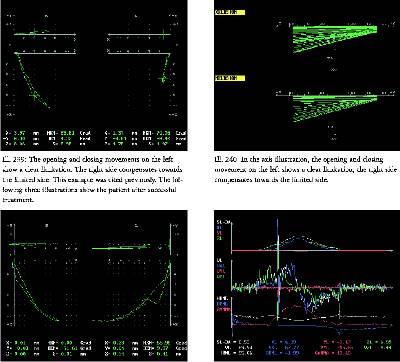
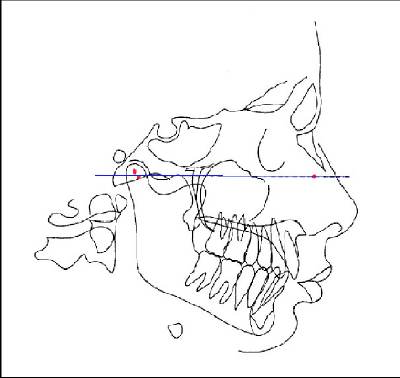
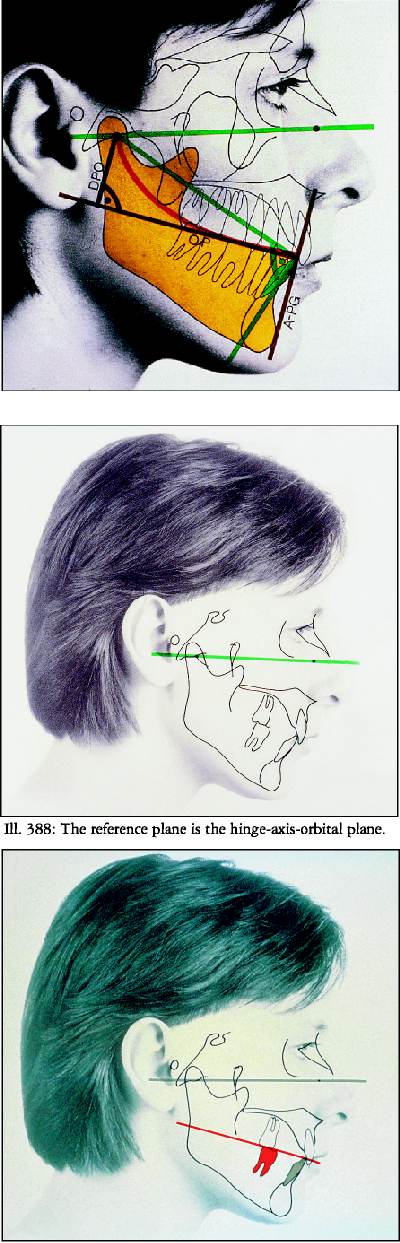
Cephalometric exam
This exam uses an X-ray of the head, where the
center of rotation of each jaw joint [shown as red dots] and a third
point are used to relate the dynamic jaw movements of the lower teeth
to all the head bones and upper teeth. This program is designed for the
placing of many digitized points from the head bones, the teeth and soft
facial tissues into a program for analyses. These analyses allow for
the determination of how the patient's spatial relationships of the head
structures relate in terms of standard deviations from norms. A big
factor is the plane of occlusion, which is the orientation of all the
teeth to the head. Deviations here cause many dysfunctional problems.
All this information can be related to the casts of the patients teeth
mounted on the articulator.
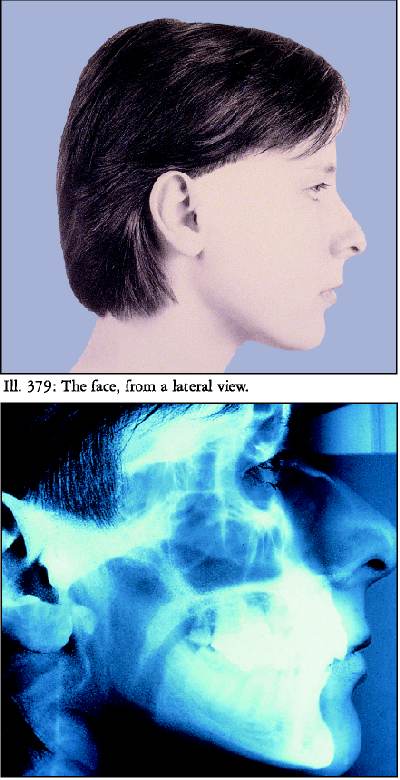
The above two pictures show the lateral view of
the patient, and the lower picture is of a lateral head film- X-ray of
the head. The computer program allows for the digitizing into a program
all the bones of the head and teeth for analyses
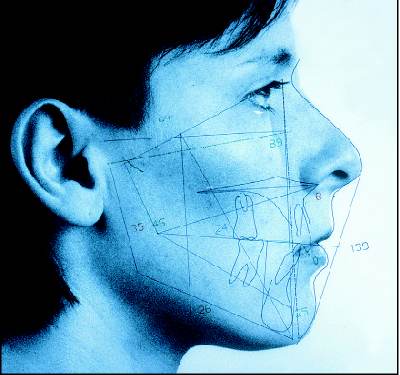
The illustration on the left shows the
computerized data from the cephalometirc program overlaid on a photo of
the patient. The numbers represent the relationships of the bones and
teeth to each other in degrees, and in further analyses these numbers
are compared to statistical norms.
TREATMENT:
After all the exams are accomplished the
results are related to the patient's symptoms in a cause and effect
process. In this context, there is too much information to be express
here due to the many factors that represent orofacial pain and
disorders, the diagnoses and proposed treatments. However, a few
examples can be given in two cases.
CASE 1
This patient complains of
headaches every morning, often during the day, and especially at
times of stress. The patient also complains of pains in the sides of
the face, difficulty opening their mouth wide, problems chewing, and
some difficulty hearing although hearing tests are near normal. The
patient's symptoms also include some dizziness, feeling tired,
and a hard time concentrating without specific effort. The patient's
history reveals that the headaches started when she reached twenty
years of age, orthodontic treatment with teeth extracted was done
during the teen years, along with academic problems in schools. The
patient points to the areas above and below the eyes and sides of the
head to show where the headaches appear.
The
muscle exam shows painful temporal tendon insertions, the muscles on
the side of the head that insert on the lower jaw used to elevate and
retrude the lower jaw. There is also a lot of pain when pressing on
the area of the lateral pterygoid muscles that move the lower jaw
forward and side to side. In this case even the insertions of the
medial pterygoid muscles is tender at the lower border of the lower
jaw.
The
posture exam shows a forward head position, and the muscles
supporting the head are painful. There is also pressure on the
examiners finger placed into the ear canal when the patient closes
the jaw. This indicates that the jaw joint is driven backward,
partially closing the ear canal, and putting pressure on the nerves
supplying the inner ear.
The
occlusal gram exam shows that the patient hits very hard on their
front teeth first, before making contact on the back teeth. This
test also shows teeth hitting on the side opposite from the side the
patient is moving their jaw. These are called balancing side
interferences, and have been known to create hyper-activity of the
medial pterygoid muscles.
In
relating the diagnostic casts of the patient's teeth to each
other from a reference position bite registration, it appears that
the lower teeth are ahead of their respective positions relative to
the upper teeth, and upon placing all the teeth together, the lower
jaw is forced backwards.
The
analyses from the cephalometric exam show that the X-rayed position
of the teeth are further back than normal positions of patient's
teeth with the same boney types and relationships of the head bones.
This indicates that the teeth are too far back in the head, creating
the problem with moving the lower jaw too far backwards when all the
teeth are together during a full bite.
The
Condylographic exam illustrates a limited mouth opening, with
otherwise normal tracings of the lower jaw's movements. There
is also a “tail” at the beginning of the tracing from the
position when the patient had their teeth together, indicating that
the jaw joint was too far back in this starting position.
The
clinical impression from the patient's symptoms and the
findings during the exams indicated that this is what is termed a
“compression case”, due to excessive pressure in the jaw
joints.
TREATMENT:
Phase 1
After
all the data is taken into consideration, the first phase of
treatment is to make a decompression splint.
A splint is a removable plastic device which covers either the upper or lower teeth to
reposition the lower jaw. Splints are divided
into 5 classical categories based on the diagnostic needs of the
patient. They are diagnostic devices, not intended for treatment;
rather they are designed to resolve the patient's immediate
problems, therefore acting as a pain management tool, and to give
guidance for future treatment. The splint is made on the diagnostic
casts of the patient's teeth to alleviate the problems found in
the exams. This splint is made on the lower teeth so the patient can
wear it all the time and still speak. Eating with the splint in is
problematical for most patients however, shortly after wearing this
splint the back teeth no longer will touch in normal closing of the
jaw. All splints are not intended to be used for more than 6 weeks,
as after six weeks if the pain resulting in symptoms is not relieved,
one must question the diagnosis.
Phase 2
Phase 2 treatment is intended for a longer term
of diagnostic evaluations,
where the entire occlusion of all teeth comes to play in the original
diagnosis, as in this case. The most suitable device to be employed
is the use of overlays that are bonded to the existing teeth, to
replace the splint. From the overlays, many treatment options are
available, to include re-doing the orthodontic treatment, simple
moving of the upper front teeth to allow the lower jaw to come
forward to later move or crown all or some of the back teeth.
Phase 3
Phase 3 is referred to as the final or
definitive stage of treatment. In
the above case example, the patient experienced frequent headaches,
and pains in and around the head and neck. The diagnostic splint
relieved these symptoms, and the results of the many exams indicated
a direct relationship between the posture of the lower jaw and the
upper jaw whereby, moving the lower jaw forward relieved the
symptoms. Definitive treatment is then directed towards moving the
upper teeth forward, either by fixed or removable orthodontic
appliances. Often in cases like this, full orthodontic treatment is
done to replace the extracted premolars, and to advance the mandible.
In cases where this is not an option due to the patient's
desires overlays can be placed, with the understanding that this is
not considered long term treatment, however the need to wear a splint
is eliminated.
CASE 2
This
patient presents with complaints of headaches, pain in and around the
head and neck, problems chewing, loss of tooth structure due to
bruxing all the time, and a lot of clicking and popping noises in
both jaw joints. The patient also complains of sleep apnea, feeling
tired all the time and listlessness.
The
muscle exam reveals pain in all the muscles moving the lower jaw, as
well as the head posture and upper back muscles.
The
occlusal gram shows that the patient has worn down the teeth to the
extent that they are in contact in all lower jaw movements. This
clearly indicates the presence of balancing side contacts, which will
prompt muscles normally intended to be relaxed to become in tension all the
time.
The
mounted casts of the patient show the amount of tooth loss from
bruxing and the machine like precision the patient has worn down the
teeth in all positions of the lower jaw.
The
Condylographic exam shows the presence of the clicking late in the
opening of the mouth at the level of each jaw joint and the presence
of the second clicking noise when the mouth is almost fully closed.
The clinical impression is that the disc that is supposed to be
between the lower jaw's condyle and the depression, or fosse,
in the head bone is displaced ahead of the head of the condyle.
Then, after the patient opens the tissues attached between the head
bone and disc are fully stretched, which moves the disc back on top
of the condyle in its normal position. However, when the patient
closes and the worn down teeth contact again, the condyle goes far
back into the fosse and the disc is pushed off the top and ahead of
the condyle. The terms for this disorder are: luxation with
reduction of the temporomandibular joint.
The
cephalometric analyses reveal that the patient's bite is
closed, the occlussal plane is flattened, and the teeth are a lot
shorter than normal.
TREATMENT
Phase 1
A
lower splint was constructed to open the patient's bite and
worn during the day time, at the position where the disc remained in
its proper place on top of each condyle as determined from the
Condylographic data as transferred to the articulator. A night time
upper splint was also made to keep the patient's bite open and
the lower jaw forward while sleeping.
Phase 2
The
diagnostic splints worn during phase 1 eliminated the headaches, and
much of the muscle pain. Physical and massage therapy was also
introduced into the treatment plan. Upper and lower splints were
then made in the ideal shapes of the patient's once existing
teeth before they were worn down from bruxing, in the position of
where the discs remained in their proper place.
Phase 3
After
many months of wearing the Phase 2 upper and lower tooth-form
splints, the patient had relief from pain and liked the appearance
these splints restored to the natural appearance. The final or
definitive treatment choice was to place crowns on all teeth to
restore the missing tooth structure, and maintain a proper posture of
the lower jaw enabling the discs to remain in their proper place.
The patient also significantly reduced the use of a machine designed
to assist breathing while sleeping. After several years of follow-up
exams, the patient remained headache and pain free.
Further
information about the approach taken in the office is available by
viewing the web-site of the Institute of Advanced Definitive
Dentistry at: www.iadd.net.
Click on: Theses/Publications, to view the many research projects
already completed and published. The Curriculum Vitae of each
dentist on the faculty at IADD is also available.
Information about the computerized data
gathering diagnostic and research instruments employed in this dental
practice is available at: www.gammadental.com.